Show
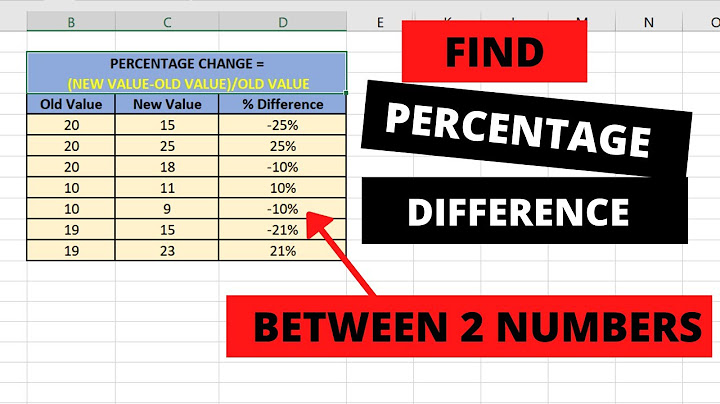
 ObjectiveTo assess correlation between blastocyst morphology and chromosomal status. DesignObservational research study. SettingAn IVF clinic and a specialist preimplanation genetic diagnosis (PGD) laboratory. Patient(s)Ninety-three couples undergoing IVF treatment in combination with chromosome screening of embryos. Intervention(s)Five hundred blastocysts underwent trophectoderm biopsy and comprehensive chromosome screening using comparative genomic hybridization (CGH). The morphology of the embryos was evaluated using standard methods. Main outcome measure(s)Association of aneuploidy and morphologic score. Result(s)A total of 56.7% of blastocysts were aneuploid. One-half of the grade 5/6 blastocysts were euploid, compared with only 37.5% of embryos graded 1/2, suggesting an effect of aneuploidy on blastocyst development. Aneuploidy also had a negative effect on inner cell mass and trophectoderm grades. Morphologically poor blastocysts had a higher incidence of monosomy and abnormalities affecting several chromosomes. The gender ratio was significantly skewed in relation to morphology. A total of 72% of blastocysts attaining the highest morphologic scores (5AA and 6AA) were found to be male, compared with only 40% of grade 3 embryos. Conclusion(s)Morphology and aneuploidy are linked at the blastocyst stage. However, the association is weak, and consequently, morphologic analysis cannot be relied on to ensure transfer of chromosomally normal embryos. A significant proportion of aneuploid embryos are capable of achieving the highest morphologic scores, and some euploid embryos are of poor morphology. Gender was associated with blastocyst grading, male embryos developing at a significantly faster rate than females. Key WordsMorphology chromosome aneuploidy blastocyst preimplantation genetic screening single embryo transfer implantation in vitro fertilization Cited by (0)Copyright © 2011 American Society for Reproductive Medicine. Published by Elsevier Inc. All rights reserved.  A common question we get asked about the process is, “How many normal (euploid) embryos will I produce?” Demko et al addressed this very issue in a recent publication. They analyzed the relationship between maternal age and the rate of embryos that tested as euploid, the average number and proportion of normal embryos per IVF cycle and the possibility of retrieving at least one normal embryo. Results of Study on Age and Number of Eggs Obtained After Preimplantation Genetic Screening The study analyzed more than 46,000 embryos between 2009 and 2014.
They concluded that (1) 33% to 50% of all embryos screened in women aged 18 to 48 years are aneuploid and (2) the number and percentage of euploid embryos decreases with advancing maternal age. At InVia Fertility Specialists, we have been offering SMART IVF (PGD or PGS) for many years. Currently, using this technology, we are having pregnancy rates approximating 70% with the transfer of a single embryo. To see a fertility specialist with a high success rate using single embryo transfer, make an appointment at one of InVia's four Chicago area fertility clinics. What percentage of embryos come back PGS normal?Patients often hear “PGS-normal embryos have a 60 – 70% success rate.” But that is on a per-transfer basis. Meaning that if you begin a cycle, retrieve eggs, produce embryos, then do PGS testing, and at least one embryo comes back normal, 60 – 70% of the time it will lead to a live birth.
What percentage of embryos are chromosomally abnormal?It may be a normal phenotype." Previous studies have reported anywhere from 4% to 90% of human embryos with mosaic chromosome counts. Such a wide range is the result of discrepant research using the most prevalent screening in IVF called "preimplantation genetic testing," or PGT.
What percentage of embryos pass PGT A?Embryo implantation rates were 66% per embryo transferred for each age group using their own eggs. One embryo screened with PGT-A produces very high pregnancy rates after transfer.
Can blastocyst have chromosomal abnormalities?Chromosomal abnormalities do not impair embryo development as aneuploidy is frequently observed in embryos that reach the blastocyst stage. High-quality blastocysts are not representative of euploidy of chromosomes 13, 14, 15, 16, 18, 21, 22, X and Y.
|

Related Posts
Advertising
LATEST NEWS
Advertising
Populer
Advertising
About

Copyright © 2024 en.apacode Inc.